Understanding Diabetes Treatment: Types, Approaches, and Innovations
Diabetes management has evolved significantly over the years, offering patients more effective ways to control blood sugar levels and improve quality of life. From traditional medication regimens to cutting-edge technologies, treatment approaches are increasingly personalized to address individual needs. Understanding the full spectrum of diabetes treatment options empowers patients to work with healthcare providers toward optimal health outcomes and reduced risk of complications.
Diabetes affects millions of people worldwide, requiring comprehensive management strategies to maintain health and prevent complications. Treatment approaches vary widely depending on the type of diabetes, individual health factors, and lifestyle considerations. Modern diabetes care encompasses medication, technology, lifestyle modifications, and ongoing monitoring to help patients achieve stable blood glucose levels and improved quality of life. As research continues to advance, new treatment options continue to emerge, offering hope for better management and potentially even cures for this chronic condition.
Understanding Diabetes: Types, Causes, and Risk Factors
Diabetes is characterized by the body’s inability to properly regulate blood glucose levels. Type 1 diabetes results from an autoimmune response that destroys insulin-producing beta cells in the pancreas, requiring lifelong insulin therapy. Type 2 diabetes, the most common form, develops when the body becomes resistant to insulin or doesn’t produce enough insulin to maintain normal glucose levels. Gestational diabetes occurs during pregnancy and typically resolves after childbirth, though it increases future risk of type 2 diabetes.
Risk factors for type 2 diabetes include family history, excess weight, physical inactivity, age over 45, and certain ethnicities. Prediabetes, characterized by higher-than-normal blood glucose levels that haven’t reached diabetic thresholds, affects millions who often progress to full diabetes without intervention. Understanding these distinctions is crucial for determining appropriate treatment approaches, as each type requires different management strategies.
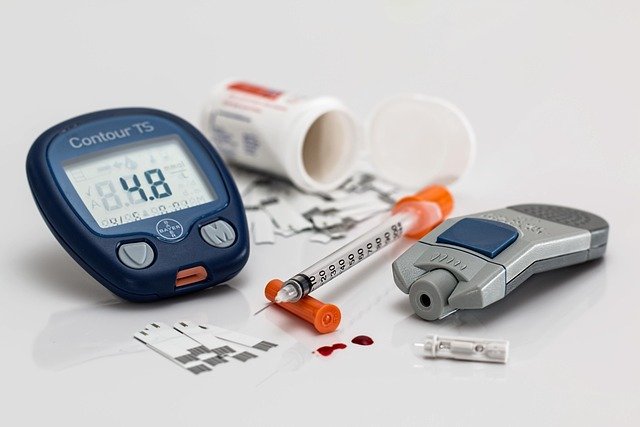
The Importance of Blood Sugar Monitoring
Regular blood glucose monitoring forms the cornerstone of effective diabetes management. For people with diabetes, tracking blood sugar levels provides immediate feedback on how food, physical activity, stress, and medication affect their glucose control. Modern monitoring options include traditional fingerstick methods and continuous glucose monitoring (CGM) systems that measure glucose levels throughout the day and night.
The frequency of monitoring depends on the type of diabetes and treatment plan. Those using insulin typically check more frequently, while some with well-controlled type 2 diabetes might monitor less often. Regular monitoring helps prevent dangerous hypoglycemic (low blood sugar) and hyperglycemic (high blood sugar) episodes. The data collected through monitoring enables healthcare providers to make informed adjustments to treatment plans, ensuring optimal glucose control and reducing the risk of long-term complications such as cardiovascular disease, neuropathy, and retinopathy.
Medication Approaches for Diabetes Management
Medication options for diabetes have expanded significantly in recent decades. For type 1 diabetes, insulin remains the primary treatment, available in various formulations including rapid-acting, short-acting, intermediate-acting, and long-acting options. Insulin delivery methods include traditional injections, insulin pens, and insulin pumps that provide continuous delivery.
Type 2 diabetes treatment often begins with metformin, which improves insulin sensitivity and reduces glucose production in the liver. Additional medication classes include sulfonylureas, which stimulate insulin release; DPP-4 inhibitors, which prevent the breakdown of incretin hormones; GLP-1 receptor agonists, which increase insulin secretion and slow digestion; SGLT2 inhibitors, which prevent glucose reabsorption in the kidneys; and thiazolidinediones, which improve insulin sensitivity. These medications may be used alone or in combination depending on individual needs and response. Treatment plans are increasingly personalized, considering factors such as cardiovascular risk, kidney function, weight management goals, and patient preferences.
Innovations in Diabetes Treatment and Technology
Technological advances have revolutionized diabetes care in recent years. Closed-loop insulin delivery systems, sometimes called artificial pancreas systems, combine CGM with insulin pumps that automatically adjust insulin delivery based on real-time glucose readings. Smart insulin pens track doses and timing, helping patients maintain consistent medication schedules.
Digital health applications now allow patients to track glucose levels, medication, food intake, and physical activity in one place, providing valuable insights for self-management. Some apps even offer predictive analytics to help prevent glucose excursions before they occur. Implantable continuous glucose monitors eliminate the need for frequent sensor changes, providing convenience and improved adherence.
Islet cell transplantation remains an experimental but promising approach for some patients with type 1 diabetes, potentially reducing or eliminating the need for insulin therapy. Smart contact lenses and non-invasive glucose monitoring technologies are under development, aiming to make glucose monitoring more convenient and pain-free for patients in the future.
Emerging Research in Diabetes Treatments and Cures
Research into novel diabetes treatments continues to advance rapidly. For type 1 diabetes, immunotherapy approaches aim to preserve remaining beta cell function by modulating the immune system’s attack. Stem cell therapies show promise for regenerating insulin-producing cells, potentially offering a functional cure for some patients.
For type 2 diabetes, dual and triple receptor agonists that simultaneously target multiple metabolic pathways are showing impressive results in clinical trials, particularly for glucose control and weight management. Researchers are also investigating the gut microbiome’s role in insulin resistance and glucose metabolism, potentially leading to novel probiotic or microbiome-based therapies.
Gene therapy approaches are being explored for both types of diabetes, with researchers working to correct genetic factors contributing to disease development or progression. While a definitive cure remains elusive, these emerging treatments offer hope for improved management and potentially disease modification or reversal for some patients.
Tips for Preventing Type 2 Diabetes in At-Risk Individuals
Prevention strategies for type 2 diabetes focus primarily on lifestyle modifications. Weight management stands as perhaps the most effective preventive measure, with research showing that losing just 5-7% of body weight can significantly reduce diabetes risk in prediabetic individuals. Regular physical activity of at least 150 minutes per week improves insulin sensitivity and helps maintain healthy weight.
Dietary approaches emphasize whole foods, including plenty of vegetables, fruits, whole grains, lean proteins, and healthy fats while limiting processed foods, refined carbohydrates, and added sugars. The Mediterranean and DASH diets have shown particular benefit for diabetes prevention. Regular health screenings are essential for those with risk factors, as early detection of prediabetes provides an opportunity for intervention before progression to diabetes.
Stress management and adequate sleep also play important roles in prevention, as chronic stress and poor sleep can affect glucose metabolism and increase insulin resistance. For those at very high risk, medications like metformin may be prescribed as preventive therapy, though lifestyle modifications remain the foundation of prevention efforts.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.