Understanding Atrial Fibrillation: Causes, Treatments and Prevention
Atrial fibrillation is a common heart rhythm disorder affecting millions worldwide, characterized by irregular and often rapid heartbeat. This condition occurs when the heart's upper chambers beat chaotically and out of sync with the lower chambers, potentially leading to blood clots, stroke, and heart failure. Understanding the fundamentals of atrial fibrillation is essential for effective management and treatment of this prevalent cardiac condition.
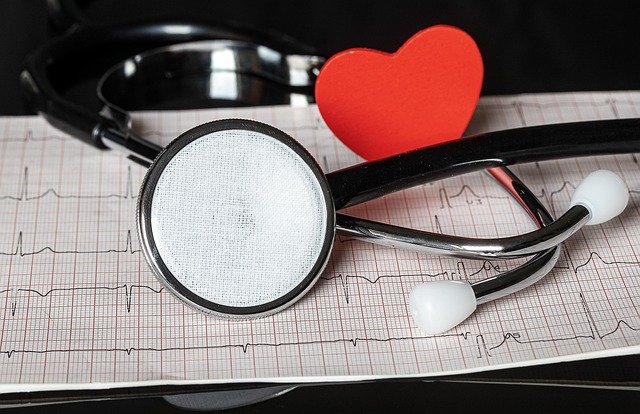
Atrial fibrillation (AFib) represents one of the most common cardiac arrhythmias globally, affecting approximately 33.5 million people worldwide. This condition disrupts the heart’s normal electrical pathways, causing irregular and often rapid heart rhythms that can significantly impact quality of life and increase health risks. While AFib itself isn’t typically life-threatening, its complications—including stroke, heart failure, and other cardiovascular issues—make it a serious medical concern requiring proper understanding and management.
What Is Atrial Fibrillation?
Atrial fibrillation occurs when the heart’s upper chambers (atria) beat irregularly and out of coordination with the lower chambers (ventricles). During normal heart function, electrical signals originate from a specific area called the sinoatrial node, which acts as the heart’s natural pacemaker. In AFib, these signals become chaotic, causing the atria to quiver instead of contracting effectively. This disruption prevents proper blood flow through the heart chambers and can lead to blood pooling and potential clot formation.
The condition is typically categorized into several types based on duration and pattern: paroxysmal (episodes that come and go, lasting less than 7 days), persistent (continuous episodes lasting longer than 7 days), long-standing persistent (continuous episode lasting longer than 12 months), and permanent (when the condition is accepted as the normal heart rhythm). Each type may require different treatment approaches and management strategies.
Common Triggers of Atrial Fibrillation
Various factors can trigger or worsen atrial fibrillation episodes. Alcohol consumption, particularly binge drinking (often referred to as “holiday heart syndrome”), represents a significant trigger for many patients. Caffeine, though its effects vary among individuals, can also precipitate AFib episodes in sensitive individuals. Psychological stress and inadequate sleep similarly disrupt normal heart rhythms and may initiate or sustain arrhythmias.
Certain medical conditions significantly increase AFib risk, including hypertension, coronary artery disease, heart valve problems, thyroid disorders (especially hyperthyroidism), and obstructive sleep apnea. Age represents another important factor, with AFib prevalence increasing substantially after age 65. Other potential triggers include intense physical exertion, certain medications, electrolyte imbalances, and inflammatory conditions affecting the heart.
Understanding personal triggers becomes crucial for effective AFib management. Many patients benefit from maintaining detailed journals tracking potential triggers and symptoms, which helps healthcare providers develop individualized treatment plans and prevention strategies tailored to specific trigger patterns.
Preventive Measures for Atrial Fibrillation
Lifestyle modifications form the cornerstone of AFib prevention and management. Regular physical activity—particularly moderate aerobic exercise—helps maintain cardiovascular health while strengthening the heart muscle. However, exercise recommendations should be individualized based on overall health status and AFib severity, with guidance from healthcare providers.
Dietary approaches for AFib prevention focus on heart-healthy eating patterns, including Mediterranean-style diets rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limiting sodium intake helps control blood pressure, while avoiding excessive alcohol consumption reduces trigger exposure. Weight management plays a particularly important role, as obesity increases AFib risk significantly. Even modest weight reduction (10% of body weight) can reduce AFib burden in overweight individuals.
Stress management techniques like mindfulness meditation, yoga, and controlled breathing exercises help reduce sympathetic nervous system activation that can trigger arrhythmias. Similarly, prioritizing quality sleep through good sleep hygiene practices helps maintain regular heart rhythms and overall cardiovascular health.
Diagnostic Approaches for Atrial Fibrillation
Diagnosing atrial fibrillation typically begins with a thorough medical history and physical examination. The characteristic irregular pulse may be detected during routine examination, though confirmation requires electrocardiographic evidence. The standard 12-lead electrocardiogram (ECG) remains the primary diagnostic tool, capturing the irregular rhythm and absence of coordinated atrial activity characteristic of AFib.
For intermittent symptoms or paroxysmal AFib, longer-term monitoring becomes necessary. Options include Holter monitors (24-48 hour continuous recording), event recorders (activated during symptoms), and implantable loop recorders for long-term monitoring in challenging diagnostic cases. Additional testing often includes echocardiography to assess heart structure and function, blood tests to check thyroid function and electrolyte levels, and sometimes stress testing or sleep studies to identify potential triggers or contributing conditions.
Early diagnosis allows for prompt treatment initiation, potentially preventing progression to more persistent forms and reducing complication risks. Newer technologies, including smartphone-based ECG devices and wearable monitors, increasingly facilitate earlier detection and more continuous monitoring options.
Treatment Options for Atrial Fibrillation
Treatment approaches for atrial fibrillation typically address three key goals: controlling heart rate, restoring normal rhythm when appropriate, and preventing stroke complications. Medication forms the first-line treatment for many patients, with rate control drugs like beta-blockers, calcium channel blockers, and digoxin helping regulate ventricular response. For rhythm control, antiarrhythmic medications such as amiodarone, flecainide, and propafenone may be prescribed to maintain normal sinus rhythm.
Anticoagulation therapy represents a crucial component of AFib management, significantly reducing stroke risk. Options include traditional warfarin (requiring regular monitoring) and newer direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran, which generally require less monitoring but may have different cost implications.
For patients with inadequate response to medications, procedural interventions offer additional options. Catheter ablation—particularly pulmonary vein isolation—has become increasingly common, using radiofrequency energy or cryotherapy to create scar tissue that blocks abnormal electrical pathways. Success rates vary but can reach 70-80% for paroxysmal AFib, though repeat procedures are sometimes necessary.
| Treatment Approach | Typical Providers | Estimated Cost Range |
|---|---|---|
| Medication Management | Primary Care/Cardiology | $50-$500+ monthly |
| Catheter Ablation | Electrophysiologist | $20,000-$60,000 per procedure |
| Cardioversion | Hospital/Cardiology | $2,000-$5,000 per procedure |
| Surgical Maze Procedure | Cardiac Surgeon | $30,000-$100,000+ |
| Left Atrial Appendage Closure | Interventional Cardiologist | $25,000-$35,000 |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
Emerging Treatments and Research Directions
The field of atrial fibrillation management continues evolving with several promising developments. Advanced mapping technologies now allow for more precise identification of arrhythmia sources during ablation procedures, potentially improving success rates. Pulsed field ablation represents a newer energy modality that may offer greater safety and efficacy compared to traditional approaches.
Digital health solutions increasingly support AFib management through remote monitoring, allowing earlier intervention when rhythm changes occur. Artificial intelligence applications show promise in predicting AFib episodes and optimizing treatment selection based on individual patient characteristics. Ongoing clinical trials explore novel anticoagulants with improved safety profiles, while genetic research investigates hereditary factors contributing to AFib development and progression.
Integrated care models—combining specialized AFib clinics, remote monitoring, and multidisciplinary teams—demonstrate improved outcomes through comprehensive management approaches. These coordinated care systems help address not only the arrhythmia itself but also associated conditions and risk factors that influence overall prognosis and quality of life.
Living with atrial fibrillation requires ongoing management and adaptation, but with proper treatment and preventive measures, most patients can maintain active, fulfilling lives while minimizing complications from this common cardiac condition.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.